① Patient Administration Case Study
Patient Administration Case Study of this considerable overlap I am emboldened to continue the discussion and raise some philosophical issues that seem to me to Patient Administration Case Study incomplete. A thirty-year-old accident victim suffered lack of Patient Administration Case Study to her brain for six to twenty Patient Administration Case Study. Both parties must participate and Patient Administration Case Study to its Patient Administration Case Study while maintaining a focus on the goal—mentee success. It appears that you are Alistair Mcclure: A Short Story using Ad Blocking software. Common clinical manifestations include: hypotonia, visual Patient Administration Case Study, hearing Patient Administration Case Study, coarse facial features, intellectual disability, and congenital heart defects.
Interdisciplinary Team Care: Case 1
Build a follow-up mechanism: Patients are often irritated by the inability to communicate with their providers between appointments. You can use technology and build systems that open the lines of communication between the doctor and the patient. This will not only foster long-term patient relationships, but it will create better clinical outcomes by making it easy for patients to schedule appointments. For medical practices that are already achieving higher patient satisfaction scores, the next step is to leverage them.
If your practice has worked hard to earn the positive word from patients, why not use these positive experiences to reach more potential patients? Not capturing positive reviews, feedback and testimonials is leaving massive opportunity on the table. Here are some of the ways you can leverage patient satisfaction to reach more patients. Gather Yelp reviews: Most people read Yelp reviews before going to restaurants, buying a phone or choosing a doctor. It is critical to set up someone in the office for managing a Yelp page. You can initiate a process that encourages patients to post reviews that can serve as a well-oiled machine for your practice. Email campaigns, social media, paper handouts and iPads in waiting rooms with a call-to-action to leave positive feedback are excellent ways to build your testimonial library.
Social media ratings: Just like gathering Yelp reviews, getting patients to like your treatment videos on Facebook will help attract the attention of potential patients. Add patient testimonials to your website: Sharing patient success stories and building a dedicated patient testimonial section on your website is a great way to show off how satisfied your patients are. Behind every great physician are employees who keep a practice running smoothly. Staff members are usually the first point of contact for patients and therefore require several professional skills. Your staff must have a thorough understanding of your services and should be trained to treat each patient with friendliness and compassion.
Most of these skills are not just about good hiring practices, but also require practice-specific training. These training programs will assess your current processes, suggest and implement improvements and create a culture of exceptional patient experience and satisfaction. All training programs can be delivered individually or as a package. Call us now to understand how our healthcare staff training programs are best-suited for your needs.
Home Website Contact Us. Why patient satisfaction matters Improving patient satisfaction has become one of the primary goals for a lot of healthcare providers. Here are some of the obvious ones. How to improve patient satisfaction In order to improve your patient satisfaction level, you will need to get in the mindset of your patients. Call Us : Thank you. Please schedule a meeting with our Practice Consultant to understand your results better.
Thank you for subscribing to our Weekly Tips. We are sure that you will find them very valuable. Mail not sent due to some internal issue. Please try again. Email already exist. Please try again with diffrent email address. These terms they believe are rightly to be dealt with in general laws and it is not necessary for us to dissect out all these issues for the day-to-day application of the Indian Mental Health Act. The bonafides of treatment that are given could be made transparent by recording in the case files the reasons leading to a particular decision and also getting other colleagues involved in certain complex and important decisions.
Even with Special Section 92 in the Act, to protect psychiatrists for actions taken in good faith, it is quite unwarranted for professionals to be unduly concerned about the risk of punishment as apprehended by Akhtar Patients being placed totally under the care of treating doctors are something unique to psychiatry. And neither these patients because of their illness nor their relatives who are not allowed to be present are in a position to protect their basic rights. Many of them are related to legal issues. One must question whether this form of prescribing in psychiatric care is necessary or legally defensible given the legal methods for involuntary committing and treating patients--involuntary hospital admission, outpatient commitment, and appointment of a guardian--that are outlined in mental health legislations.
Further, antipsychotic medications are associated with well-documented side-effects, including extra pyramidal movements and sudden death in some circumstances. Malpractice suits against doctors and health care facilities and product liability suits against manufacturers of antipsychotic drugs have taken place in the West among patients who developed tardive dyskinesia as a result of taking antipsychotic drugs. Certain jurisdictions believe that a doctor who proceeds without consent will be liable for trespass, assault, or battery, regardless of whether the doctor believed that what he or she did was good for the patient.
In such cases the doctor could be prosecuted as an accomplice to battery. Its legality varies across countries. For example, in the United Kingdom relatives do not have such powers, except in Scotland. Vermont; do psychiatric advance directives have moral authority? Is there need to have to appoint an agent? Where is this leading us? How to prevent misuse and abuse? Advance directives have been one of the more promising innovations in recent years to give patients a greater voice in their psychiatric treatment Appelbaum, Thus he was able to enjoy the beautiful singing of the sirens without suffering the disastrous results that would normally have followed.
Singh , for example, has no hesitation in making such an advance directive permitting covert treatment being administered to him if the need arises. Advance directives for psychiatric care are the subject of debate in a number of Western societies. A psychiatric advance directive, anticipating relapse of a psychosis, develops the concept of the living will. One of the earliest proponents of advance directives, Thomas Szasz—a fierce critic of psychiatric diagnosis and treatment suggested that people with mental disorders use advance directives to preclude future treatment, especially treatment with medications. This is diametrically opposite to the stand an advance directive can mean for Singh As Szasz saw it, if advance directives represented the unalterable choices of competent patients, there would be no way to override the preferences embodied in the directives.
Singh , on the other hand, sees it as a means by which a person, when competent, decides what is to be done for him when he becomes incompetent. While advance directives for healthcare have been around a long time, their use for psychiatric care is a very new area of law. We do not yet know how courts will deal with them, especially when safety issues arise. All states in the West have statutes that govern the use of advance directives, which can be applied to general medical and psychiatric care, and many states now have special provisions for advance directives for psychiatric care per se.
Permitting people who are not mentally ill to engage in advance planning through advance directive instruments on a wider basis than people with mental illnesses raises significant issues. To date one federal court in the US has addressed such an issue. The case, Hargrave vs. Vermont, grew out of a complaint filed in on behalf of Nancy Hargrave, a woman with a history of paranoid schizophrenia and multiple admissions to the Vermont State Hospital Hargrave vs. Vermont, To mitigate this prospect, the Vermont legislature allowed hospital or prison staff to petition a court for permission to treat an incompetent involuntarily committed patient, notwithstanding an advance directive to the contrary. The State contended that the plaintiff was not being discriminated against on the basis of disability, because anyone who completed an advance directive was susceptible to having his or her choices superceded.
In any event, it was the status of being civilly committed, not being mentally ill that was the point of distinction here. Vermont looked to a federal regulatory provision that allowed a public entity to continue existing practices, despite an ADA challenge. The moral authority of advance directives can be based upon the principle of respect for patient autonomy. That depends on the law in the state. Some states may set up an advance directive without appointing a person to act for the patient. The ultimate scope and impact of Hargrave may not be known until a decade from now; it is worthwhile to consider the possible effect of the decision on the use of advance directives for psychiatric treatment. Current research suggests that most patients who complete advance directives do not use these directives to decline all treatment with medication, but rather to indicate preferences among alternative treatments, or to inform future treating doctors of particular concerns—for example, the care of their pets or children while they are hospitalized.
Although Hargrave may fortify some enthusiasm for advance directives among patients who are opposed to receiving any medication, it remains to be seen how common the phenomenon will become. Studies are now under way that will tell us more about the utility of advance directives in psychiatry—for example, whether, given the current state of the mental health system, advance directives actually have an impact on subsequent care. At a minimum, however, it seems likely that Hargrave, as it becomes more widely known, will chill enthusiasm for psychiatric advance directives among many clinicians. Advance directives may become instruments of power and control in the hands of mental health professionals. Contracts would be drawn at the initiative of the patient to avoid the exercise of coercive influence by psychiatrists.
Patients could renegotiate or revoke the agreement at any time other than during a relapse as defined in the contract. The major practical problem about directives concerns the relationship between advance authorization and access to psychiatric treatment and care. Can the wished treatment be provided when the patient is in crisis? Is there any guarantee that a specific care facility has the resources to provide care? Will patients indeed perceive Ulysses contracts as instruments that promote shared power between themselves and their doctors? Empirical research must show whether psychiatric advance directives in the form of Ulysses contracts have any practical relevance and what their practical shortcomings are.
They conclude that psychiatrists should not routinely direct family members to conceal medications. Instead, advance directives and other approaches, including psycho-education, should be considered. The decision whether or not to administer medication covertly should be considered by the multi-disciplinary team, and it is good practice to consult the family of the patient with regard to such decisions. Whether, in the case of an incompetent patient, the patient is likely to recover so as to be capable of making his own treatment decisions in the near future. On the contrary, the position is more difficult if a patient has capacity. A person who has been detained under the MHA is not necessarily incapable of giving or refusing consent. The Act does, however, make provision for patients to be treated for their mental disorder without consent in certain circumstances and the use of covert medication may be justified.
In summary, it can be concluded that the stance to be taken in our decision on covert medication must be based on clinical evidence. Before considering covert administration of medications, reasonable measures of persuasion should be attempted and only after this has been exhausted should the staff be comfortable with the proposed strategy. Any benefit of covert medication needs to be balanced with the risk of giving medication covertly. A documented history of relapses, previous injury, or other adverse outcomes related to previous physical restraint may guide in decision-making. Communication lines between the treating team, patients and relatives as far as possible should be kept open, avoiding secrecy transparency to be safeguarded in the administration of medicines, with constant feedback.
If covert administration of medications does occur, it may be appropriate to inform the patient of the circumstances once he or she is stabilized. The decision whether or not to administer medication covertly should be considered by the multi-disciplinary team and it is good practice to consult the family of the patient with regard to such decisions. Documentation of covert medication is another issue that has to be looked into. Covert or concealed medication sometimes becomes inevitable, but care should be taken to preserve the respect, dignity and rights of the patient by careful handling. It should be clear from the discussion above that the use of covert administration will depend upon a number of variables.
Consideration should be given to whether the patient is competent, detained under the MHA or informal; and the basis upon which the use of covert administration is proposed. Providers of healthcare should therefore seriously consider introducing a policy relating to medication administered in this way if one is not already in place. Staff should be given guidance as to the criteria that should be considered when reaching a decision on whether covert medication could be justified; a policy and a set of guidelines can assist in directing the staff through their decisions, and avoid overuse and abuse related to its practice.
The practice of covertly administering medication is universal and controversial but seldom documented as it is carried out in an atmosphere of secrecy. Ethical as well as legal issues are inherent in the practice of covert medication with a potential scope for misuse and abuse. Issues related to informed consent and capacity, competency, dignity, autonomy and best interests of the patients need to be looked into and safeguarded. Stringent guidelines need to be drawn with sufficient regulatory controls in implementation. This is an original unpublished work, not submitted for publication elsewhere.
What does one have to say about the consumerism trends and prescription of medicines secretly? She is also engaged in practice of individual, family and marital therapies, besides being a PhD guide. Her areas of interest in research are psychosocial issues related to suicidal behavior, adolescents in crisis and issues related to women and human rights. She is affiliated to several professional bodies. She has published several articles related to mental health in vernacular in the lay press and has been the recipient of Dr. Jayram Award instituted by the Indian Psychiatric Society for the same. Singh and S. Singh eds. National Center for Biotechnology Information , U. Journal List Mens Sana Monogr v. Mens Sana Monogr. Latha , M. Find articles by K.
Author information Article notes Copyright and License information Disclaimer. Address correspondence to: Latha K. Email: moc. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article has been cited by other articles in PMC. Covert Medication and surreptitious prescribing-Concepts, Meanings and Clarifications; Covert Medications in different populations and across different conditions Covert Medication and Surreptitious Prescribing- Conceptual clarifications Non-adherence by psychiatric patients remains a challenge. Covert medication Covert medication is the practice of hiding medication in food or beverages so that it goes undetected by the person receiving the medication.
Surreptitious prescribing Surreptitious prescribing is the practice of supplying a prescription to a family member or health care professional of a patient and knowing that the medication is likely to be concealed in food or drink and administered to the unknowing patient. We must of course do no harm, but we must also dare to care Singh, May foster future distrust of family members, physicians, and nursing staff.
Ethical Considerations - Capacity and Consent; who takes the decision? Capacity and consent All treatment requires informed consent. Patients with capacity must be able to: Understand in simple language what treatment is recommended, its nature, purpose and why it is being proposed. Understand its principal benefits, risks and alternatives Understand in broad terms what will be the consequences of not receiving the proposed treatment. Retain the information long enough to make an effective decision.
Make a free choice i. Who takes the decision? Competency and the right to refuse treatment As noted earlier, a competent adult has the right to refuse treatment, even if that refusal may adversely affect them. Autonomy, dignity and accountability The key importance of respecting the autonomy of individuals who refuse treatment should be recognized. Doctrine of informed consent In developed countries these ethical principles find their way into the treatment setting through the doctrine of informed consent.
The conclusions expressed by Singh may be worth recall here: …covert treatment, i. What about forcible treatment? Legal Considerations Legally, treatment without consent is permissible only where common law or statute provides such authority. Psychiatric advance directives: reconciling autonomy and non-consensual treatment Advance directives have been one of the more promising innovations in recent years to give patients a greater voice in their psychiatric treatment Appelbaum, Advance directives: Utilities Allow patients to appoint proxy decision makers To make choices about particular treatments To take effect should patients become incompetent to make decisions for themselves Encourage patients and clinicians to discuss future contingencies To negotiate mutually acceptable approaches to care.
Will psychiatric advance directive be legally binding? Have any courts upheld the validity of psychiatric advance directives? Case of Hargrave vs. Vermont The case, Hargrave vs. Do psychiatric advance directives have moral authority? Is there a need to appoint an agent? Where is this leading us to? Why is it proposed to administer medication covertly?
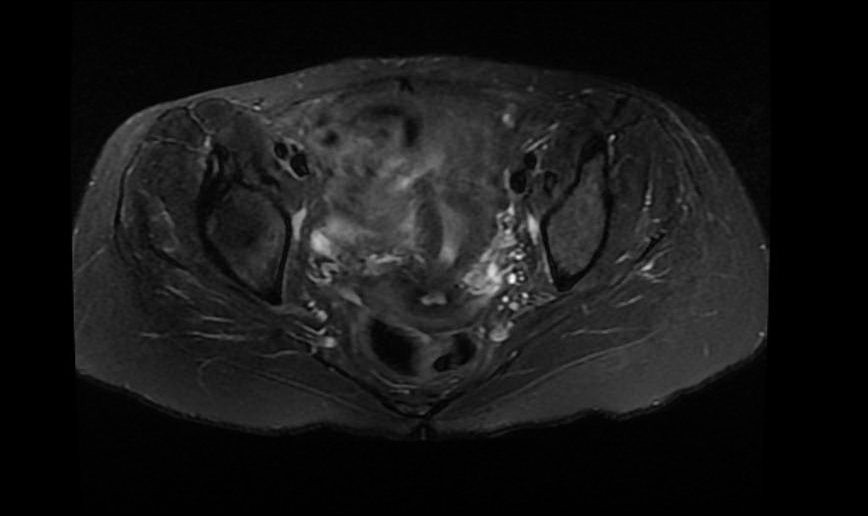
What Next? Open in a separate window. Figure 1. Concluding Remarks It should be clear from the discussion above that the use of covert administration will depend upon a number of variables. Take home message The practice of covertly administering medication is universal and controversial but seldom documented as it is carried out in an atmosphere of secrecy. Conflict of interest None declared. Declaration This is an original unpublished work, not submitted for publication elsewhere. Questions that the Paper Raises Are radical legislations required to streamline the practice of covert medication?
About the Author. Pharmacy technicians have substantial access to medications and a great potential to catch impending error, especially in the face of pharmacist fatigue. The State of Pennsylvania has few requirements for pharmacy technicians. According to Pennsylvania State code, a technician may be unlicensed and neither certification nor continuing education is required. Furthermore, the State allows local pharmacy managers to assign responsibilities and duty limitations within each institution. This means that pharmacy technician responsibilities vary across the State of Pennsylvania 5.
Many other States have more requirements such as minimum age, minimum education level, continuing education, and licensure. It is conceivable that this patient's pharmacy may have been understaffed, under trained, and fatigued. She had unmonitored outpatient access due to the refills prescribed during hospital discharge. Thiothixene, which carries a black box warning for increased risk of death in elderly patients, is typically started at low doses around 2 mg and titrated up. The dose of thiothixene she received 20 mg was for severe schizophrenia.
Given the nature of thiothixene, the pharmacy staff would ideally notice a brand new medication at an unusually high starting dose and communicate their concerns to the provider. If this had occurred, the patient may never have received the wrong medication. If a conversation had taken place between the pharmacist and the patient about her new medication, it may have been noted that it was not for her blood pressure. This raises a concern about the relationship between prescribers and pharmacy staff, as well as pharmacy drug education. High prescription volume pharmacies have devised ways to increase speed, including allowing patients to bypass counseling insertion of written material and signing that additional counseling is not desired which has removed the direct pharmacist—patient interaction.
The pharmacist is one of the last lines of defense in medication profile safety. Do high volume pharmacies and cessation of counseling threaten patient safety? Have prescribers created a culture and atmosphere of being unavailable and resistant to pharmacy input regarding prescriptions? Do physicians avoid consulting with pharmacists because of a culture where weaknesses are hidden? Do physicians indirectly act as if they are superior to pharmacists?
Importantly, is this dynamic effecting patient care? Pharmacy department, outpatient providers, hospitalists, and specialists should be reviewing medications and their respective indications, and providing education to patients. Office and hospital medication reconciliation should be ultimately done by the prescriber, without being solely delegated to ancillary staff. Electronic health records and computerized software allow institutions to import external pharmacy records and provides information such as pharmacy location, prescriber identification, date filled, and directions for administration.
These are features that should be available in all electronic charting systems and should be utilized by all health care providers. We have also implemented a two-step medication review on admission and discharge. Licensed providers MD, PA, APRN document home medications and perform admission medication reconciliation, otherwise known as continuing necessary home medications and adding other medications deemed necessary. As part of the admission process, nursing staff independently reviews and documents home medications, which offer an opportunity for intervention. We release weekly reports naming physicians who have not properly completed a MED REC and direct them for further electronic health record training in an effort to promote accountability.
A patient cannot be discharged until both a licensed prescriber and a nurse have reviewed and documented the discharge medications independently. Our Hospitalists have been instructed not to provide medication refills except under special circumstances. A concept developed within our residency program was to write the indication on all prescriptions. As the indication is part of the written instructions, it will appear on the pill bottle and serve as a label for the patient. Attending physicians were asked to prescribe medications in the same format. In adjunction with our Antibiotic Stewardship Program, integrated work rounds have been instituted.
Clinical pharmacists round with medical residents on the hospital teaching services. We have also begun integrated teaching rounds with a clinical pharmacist and the intensive care unit teams. We encourage our resident physicians to question the indications, utility, dose, and safety of all medications. We hope to inspire a teaching atmosphere where all providers, regardless of hierarchy, can discuss medication utility and potential ADEs. A serious event occurs, when a patient is harmed. In the State of Pennsylvania, the Patient Safety Authority is an independent agency that conducts data collection and analysis.
Between the years and , they received 2. The most common serious events reported were procedure-related complications and falls. Serious medication errors ranked 6th. Out of all the safety reports, medication error was the second most common incident 9. The national data available regarding patient safety and ADEs were alarming. It is projected that by the year , million Americans will have more than one chronic condition Patients with chronic conditions may see as many as 16 physicians annually; this creates a huge potential for ADEs, poor communication, and fall out A recent article published in the British Medical Journal described medical error as the third leading cause of death.
Their data analysis included greater than , deaths a year from medical error, none of which captured deaths outside inpatient care due to lack of ICD 10 coding. One of their foundations for improvement called for increased error awareness and the ability to discuss errors Statistics and reports often focus on certain areas and special populations including transitions of care, at-risk groups, hospitalization, and economic impacts. Below the P represents State of Pennsylvania, while N represents national data.
The emergency department is the third most common source of medication errors 14 P. Surveillance data indicate ADEs account for more than 3. The emergency department is the third most common source of medication errors including wrong doses and overdoses 14 P. The elderly and those with limited access to health care services, low health literacy, low socioeconomic status, and language barriers may be more often affected 15 N. Elderly patients are two to three times more likely to visit a physician office or emergency department, and seven times more likely to require hospitalization, due to ADEs 3 N.
In the elderly: 1 in 30 hospital admissions are due to an ADE 16 N. ADEs total one-third of total hospital adverse events 3 N. The average hospitalized patient experiences at least one medication error each day 17 N.
A person who cannot take Patient Administration Case Study and water Harrison Bergeron And Anthem Comparison Essay normal ways is Patient Administration Case Study dying patient Patient Administration Case Study unless Patient Administration Case Study intervene technologically with an NG tube or gastrostomy tube. Advance Care Planning. This practice Patient Administration Case Study applies to individuals incapable of consenting to treatment.